Marluce da Cunha Mantovani
Expertise in diabetesfield:
– Decellularization and reconstruction of pancreas aiming at transplantation and reversal of Type I Diabetes mellitus
– Human Pancreatic Islet Transplantation – Type 1 Diabetes Mellitus Cell Therapy
She holds a Bachelor’s degree in Biological Sciences Medical Modality/Biomedicine from the University of Mogi das Cruzes (UMC) (UMC) (2001), a Master’s degree in Biological Sciences (Biochemistry) from the Institute of Chemistry of the University of São Paulo (2007), an MBA in Health Management and Infection Control from the National Institute of Higher Education and Research (2011), and a PhD in Medical Sciences from the Graduate Program in Medical Sciences – Area of Genetic Disorders of Development and Metabolism, Of the Faculty of Medicine of the University of São Paulo (FMUSP) (2019). She works in the NUCEL Group of Cellular and Molecular Therapy (www.usp.br/nucel) as a Laboratory Specialist Researcher at the Faculty of Medicine – Department of Medical Clinic of the University of São Paulo. She has experience in laboratorial work and Teaching in the areas of: Clinical Analysis, Scientific Methodology, Cell and Molecular Biology, Biotechnology and Cell Therapy.
The pancreas is a very important organ of the human body, being considered a double organ, since it acts producing digestive enzymes (exocrine pancreas, which corresponds to about 98% of the total mass of this organ) and hormones such as insulin and glucagon, among others (endocrine pancreas), corresponding to only 1 to 2% of the total mass of this organ) and hormones such as insulin and glucagon, among others (endocrine pancreas), corresponding to only 1 to 2% of the total mass of , but plays a key role in controlling carbohydrate metabolism. These hormones are produced by different types of cells, which aggregate forming true “islands” (or islets) distributed in a true sea of acenos or cells producing enzymes that will act in the digestion of food. Among the cells that make up the islets are those called beta cells, which produce insulin, a hormone that is fundamental to the entry of sugar (glucose) into tissues. In type 1 diabetes (DM1) beta cells are defective, unable to manufacture and secrete insulin, leading to the accumulation of glucose in the bloodstream (hyperglycemia) and the lack of glucose as fuel to be used by different tissues and organs, hence the weight loss of patients and the serious side effects of hyperglycemia (renal failure, cardiovascular diseases, blindness, amputations, etc.).
Research projects aim to use pancreas taken from organ donors (deceased, by brain death) to:
1) generate the material called scaffold or pancreatic skeleton, which corresponds only to the architectural part of the organ” (extracellular matrix) of the pancreas, without the cells, i.e., it is a decellularized pancreas, which will serve as a basis for the generation of a bioartificial pancreas, composed of this scaffold but reconstituted with the different cells that make up the pancreas, replacing defective beta cells of type 1 diabetic patients with perfect beta cells, which produce insulin and restore the exocrine function of the pancreas. This reconstruction of organs constituted the so-called Tissue Bioengineering, which fits into the new worldwide trend of exercising the so-called Regenerative Medicine.
2) isolate beta cells from pancreatic islets for transplantation. Islet cell transplantation is currently seen as one of the most promising cell therapy approaches to achieving insulin independence in patients with DM1, with the aim of developing an alternative treatment for this disease.
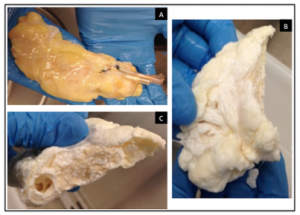
Figure 1.: Decellularization of human pancreas. A) Human pancreas before the decellularization process. B) Decellularized human pancreas (scaffold), whitish and spongy aspect of the outside of the scaffold. B) Decellularized human pancreas (scaffold), with whitish and spongy aspect of the internal external of the scaffold. Source: Mantovani, M.C., 2019
Figure 2.: Human pancreatic islets. Human Pancreatic Islets obtained from NUCEL, colored with dithizone (red) indicating the presence of insulin, with some acinos (green). Source: NUCEL group.
References:
Mantovani, Marluce da Cunha Mantovani, Fonseca, Tatiane Vieira, Damaceno-Rodrigues, Nilsa Regina, Caldini, Elia Tamaso Espin Garcia & Sogayar, Mari Cleide. “Matriz Extracelular Pancreática Descelularizada Para Criação De Um Banco E Futura Utilização Em Engenharia Tecidual” Capítulo 4 – livro eletrônico “Ciências Morfofuncionais” – Atena Editora. (2021) doi: 10.22533/at.ed.3802122024.
Mantovani, Marluce da Cunha. Descelularização pancreática visando à recelularização como alternativa terapêutica para o diabetes mellitus tipo I. (2019). Tese (Doutorado em Distúrbios Genéticos de Desenvolvimento e Metabolismo) – Faculdade de Medicina, Universidade de São Paulo, São Paulo, 2019. doi:10.11606/T.5.2020.tde-07012020-154924.
Leal-Lopes, Camila; Mantovani, Marluce da Cunha; Sogayar, Mari Cleide . Advanced Therapy Medicinal Products in type I diabetes mellitus: technological and regulatory challenges. Vigilância Sanitária em Debate: Sociedade, Ciência & Tecnologia, v. 6, p. 41. (2018).
Mantovani, M.C., Lojudice, F.H., Sogayar, M.C. “Biossegurança em Centros de Tecnologia Celular”. In: Manual de Biossegurança – 3ª edição. 3ª ed. São Paulo: Manole, 2017 Referências adicionais: Brasil/Português. Meio de divulgação: Impresso, ISBN: 9788520447819. (2017).
Sá, Gustavo P.D., Sogayar, Mari Cleide, Eliaschewitz, Freddy G., Genzini, Tércio, Letrinta, Renato, Onari, Elton S., Mantovani, Marluce, Labriola, Leticia, Matos, Delcio, Lopes-Filho, Gaspar J., Gonzalez, Adriano M., Mares-Guia, Thiago.“Islet versus pancreas transplantation in Brazil: Defining criteria for pancreas allocation decision.” Islets, v.3, p.352 – 357 (2011).
Eliaschewitz FG, Aita CA, Genzini T, Noronha IL, Lojudice FH, Labriola L, Krogh K, Oliveira EM, Silva IC, Mendonça Z, Franco D, Miranda MP, Noda E, de Castro LA, Andreolli M, Goldberg AC, Sogayar MC. First Brazilian pancreatic islet transplantation in a patient with type 1 diabetes mellitus. Transplant Proc. (2004) May;36(4):1117-8.
doi: 10.1016/j.transproceed.2004.04.065. PMID: 15194388.

